Management of brain metastases in melanoma: What should a patient know
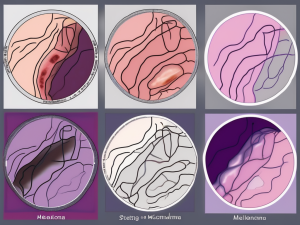
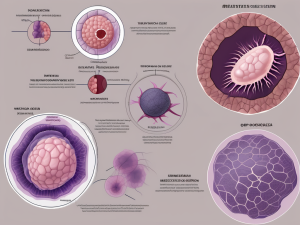
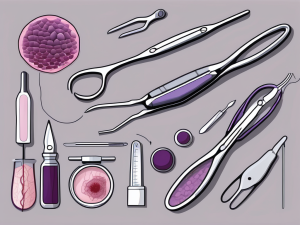
If you’re facing the journey of melanoma with the added challenge of brain metastases, this blog offers crucial insights and hope. It delves into understanding how melanoma cells can travel to the brain, emphasizing the importance of early detection and personalized treatment options. With advancements in surgery, radiation therapy, targeted therapies, and immunotherapy, there’s