Advanced Prostate Cancer Treatment: A Comprehensive Guide
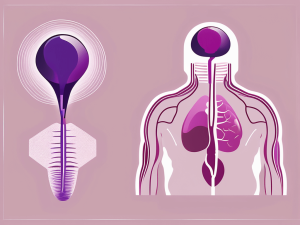
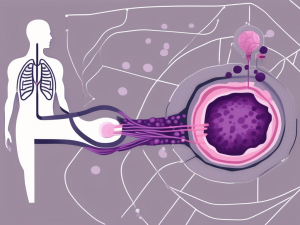
Navigating advanced prostate cancer involves understanding its progression beyond the prostate gland and exploring various treatment options. This comprehensive guide highlights that early detection is key, but for advanced stages, treatments like hormone therapy, chemotherapy, radiation, and immunotherapy are tailored to manage symptoms and improve life quality.