If you’re facing the journey of melanoma with the added challenge of brain metastases, this blog offers crucial insights and hope. It delves into understanding how melanoma cells can travel to the brain, emphasizing the importance of early detection and personalized treatment options. With advancements in surgery, radiation therapy, targeted therapies, and immunotherapy, there’s a comprehensive approach to tackling this complication. The blog also highlights the significance of supportive care in enhancing quality of life, managing symptoms, and maintaining a positive outlook. It’s a testament to the power of knowledge, the importance of a solid support system, and the advancements in medical science that offer hope for those navigating this difficult path. Let this guide be a beacon of hope and a source of invaluable information for patients and their loved ones.
If you or a loved one has been diagnosed with melanoma, it’s important to be aware of the potential for brain metastases. While this can be a challenging and overwhelming situation, understanding the basics and knowing your treatment options can help you navigate through this journey with knowledge and hope.
Understanding the Basics of Brain Metastases in Melanoma
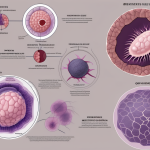
Brain metastases occur when cancer cells from the melanoma spread to the brain. This can happen through the bloodstream or through direct extension from nearby tissues. The process of cancer cells traveling to the brain is known as metastasis, and it is a complex and intricate process that involves multiple steps.
When melanoma cells break away from the primary tumor, they can enter the bloodstream or lymphatic system, allowing them to travel to other parts of the body. Once in the bloodstream, these cells can be carried to various organs, including the brain. However, not all melanoma cells that reach the brain will form metastases. The brain has a unique environment that can either promote or inhibit the growth of cancer cells.
Once the melanoma cells reach the brain, they face several challenges. The blood-brain barrier, a protective barrier that separates the brain from the bloodstream, can prevent the entry of cancer cells into the brain. However, some melanoma cells have the ability to bypass this barrier and invade the brain tissue. Once inside the brain, these cells can form new tumors, known as brain metastases.
Brain metastases are a serious complication of melanoma that requires prompt attention and treatment. They can cause a range of symptoms, depending on their size, location, and number. Common symptoms include headaches, seizures, changes in vision, difficulty speaking or understanding language, and weakness or numbness in certain parts of the body.
It is important to know that not all melanoma patients will develop brain metastases. However, if you have been diagnosed with stage IV melanoma or if your melanoma has spread to other parts of the body, you may be at a higher risk. Regular monitoring and imaging tests can help detect brain metastases early, allowing for timely intervention and treatment.
Treatment options for brain metastases in melanoma may include surgery, radiation therapy, targeted therapy, immunotherapy, or a combination of these approaches. The choice of treatment depends on various factors, such as the size and number of metastases, the overall health of the patient, and the presence of other metastatic sites.
Advancements in medical research have led to significant improvements in the management of brain metastases in melanoma. Researchers are continuously exploring new treatment strategies and developing innovative therapies to target and eliminate cancer cells in the brain. Clinical trials are also underway to evaluate the effectiveness of novel drugs and treatment combinations.
In addition to medical interventions, supportive care plays a crucial role in the management of brain metastases. This may include symptom management, psychological support, and rehabilitation services to improve quality of life and overall well-being.
Overall, understanding the basics of brain metastases in melanoma is essential for patients, caregivers, and healthcare professionals. By staying informed about the latest advancements in treatment and supportive care, individuals affected by brain metastases can make informed decisions and actively participate in their treatment journey.
The Importance of Early Detection and Diagnosis
Early detection and diagnosis of brain metastases are crucial. Regular check-ups, routine screenings, and immediate reporting of any new or worsening symptoms to your healthcare team can help in catching any potential brain metastases at an early stage.
Common symptoms of brain metastases include persistent headaches, seizures, cognitive changes, balance problems, and difficulties with speech or vision. It is essential to communicate any new or ongoing symptoms effectively with your healthcare team to ensure prompt evaluation and diagnosis.
Treatment Options for Brain Metastases in Melanoma
When it comes to treating brain metastases in melanoma, there are several options available. The most appropriate treatment plan will depend on various factors such as the number and size of the metastases, your overall health, and your treatment goals. Your healthcare team will work closely with you to develop a personalized treatment approach.
Treatment options may include surgery, radiation therapy, targeted therapies, immunotherapy, or a combination of these approaches. The specific treatment plan will be determined based on your individual needs and preferences.
Surgical Interventions: Exploring the Possibilities
Surgery may be an option for removing brain metastases, especially if they are small and localized. The procedure aims to remove the tumors while preserving brain function. Your neurosurgeon will evaluate the size, location, and accessibility of the metastases to determine if surgery is a viable option.
In some cases, minimally invasive techniques, such as laser ablation or stereotactic radiosurgery, may be used to precisely target and treat the metastases. These procedures offer the advantage of shorter recovery times and reduced risk of complications.
Radiation Therapy: A Promising Approach for Brain Metastases
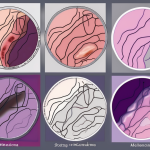
Radiation therapy involves using high-energy beams to destroy cancer cells in the brain. It can be delivered externally (external beam radiation therapy) or internally (brachytherapy).
External beam radiation therapy is a non-invasive treatment that delivers radiation from outside the body. It is typically administered in multiple sessions over a few weeks. Brachytherapy, on the other hand, involves placing radioactive material directly into the tumor. This localized approach allows for a higher dose of radiation to be delivered while minimizing damage to surrounding healthy tissue.
Targeted Therapies: Revolutionizing Melanoma Treatment
Targeted therapies are medications that specifically target the abnormalities in cancer cells. These drugs work by interfering with the growth and spread of melanoma cells. Some targeted therapies have shown promising results in treating brain metastases in melanoma.
Targeted therapies can have different mechanisms of action, such as blocking specific proteins that drive cancer growth or stimulating the immune system to attack cancer cells. Your healthcare team will assess the specific genetic mutations in your melanoma and determine if targeted therapies are suitable for your treatment plan.
Immunotherapy: Harnessing the Power of the Immune System
Immunotherapy has revolutionized the treatment of melanoma. These medications work by enhancing the body’s own immune system to recognize and destroy cancer cells, including those that have spread to the brain.
Checkpoint inhibitors, a type of immunotherapy, have shown significant success in treating melanoma with brain metastases. These drugs release the brakes on the immune system, allowing it to effectively attack cancer cells. Immunotherapy can be a promising option for patients whose melanoma does not have specific genetic mutations targeted by other therapies.
Managing Symptoms and Side Effects: A Comprehensive Guide
Managing symptoms and side effects is an integral part of the overall treatment plan. Your healthcare team will work with you to develop strategies to minimize discomfort and improve your quality of life.
Common symptoms and side effects of brain metastases treatment may include fatigue, hair loss, nausea, and changes in appetite. Additionally, treatment for brain metastases can sometimes cause neurological symptoms, such as headaches or memory difficulties. Open communication with your healthcare team is vital to address and manage these symptoms effectively.
Supportive Care: Enhancing Quality of Life for Patients
Supportive care focuses on improving the overall well-being of patients facing brain metastases in melanoma. This approach encompasses a wide range of services designed to address physical, emotional, and practical needs.
Supportive care can include pain management, psychological support, nutritional guidance, and assistance with everyday tasks. It is crucial to have a strong support system in place, including family, friends, and healthcare professionals who can guide you through this challenging time.
Prognosis and Long-Term Outlook: What to Expect
Understanding the prognosis and long-term outlook for brain metastases in melanoma can be both daunting and important. Every individual’s journey is different, and prognosis depends on various factors.
Advancements in treatment options have improved survival rates and quality of life for patients with brain metastases in melanoma. Collaborate closely with your healthcare team, follow your treatment plan diligently, and maintain a positive mindset. There is always hope for better outcomes, and ongoing research continues to bring promising advancements in the field of melanoma treatment.
In conclusion, managing brain metastases in melanoma requires a comprehensive understanding of the disease and its treatment options. Early detection, timely diagnosis, and a personalized treatment plan are key to optimizing outcomes. Remember that you are not alone in this journey; rely on your healthcare team, and lean on your support network to navigate through the challenges with courage and hope.