Telehealth is revolutionizing oncology by providing unprecedented access to cancer care, especially for those in remote or underserved areas. This blog post explores how digital technologies are transforming the patient experience, from facilitating virtual consultations with oncologists to enabling remote monitoring and follow-up care. It highlights the empowerment of patients through active participation in their health management and the expansion of access to clinical trials via tele-trials. Despite facing challenges like privacy concerns and the digital divide, telehealth in oncology promises to enhance patient outcomes, reduce barriers to care, and pave the way for a more accessible and efficient healthcare landscape.
In the dynamic world of healthcare, telehealth has emerged as a strong frontier of innovation, particularly in oncology. This digital revolution is not just changing the game; it’s redefining it, offering new hope and unparalleled access to care for cancer patients around the globe. This blog post shines light on the transformative impact of telehealth on cancer care, its benefits, the empowerment of patients through remote monitoring, and the future it heralds for diagnosis and clinical trials.
Telehealth: A New Frontier in Cancer Care
Telehealth, or telemedicine, leverages digital communication technologies to deliver healthcare services remotely, connecting patients and healthcare professionals in ways previously unimaginable. In oncology, this has been nothing short of revolutionary. Patients, irrespective of their location, now have timely and convenient access to specialized care, breaking down barriers that once made world-class cancer treatment a distant dream for many.
For those in rural or underserved regions, the journey to a cancer center can be daunting, marked by long distances and the physical and emotional toll of travel. Telehealth eliminates these obstacles, offering virtual consultations with leading oncologists and ensuring that expert advice is just a video call away.
Beyond consultations, telehealth’s scope extends to remote monitoring and follow-up care. Wearable devices and digital platforms enable oncology teams to keep a real-time check on patients’ vital signs, medication adherence, and side effects, fostering a proactive healthcare environment that prioritizes patient safety and comfort.
Empowering Patients Through Remote Monitoring
The advent of remote monitoring technologies marks a significant stride in patient empowerment. Cancer patients can now monitor their health metrics and symptoms from home, actively participating in their care. This not only bolsters patient engagement but also ensures early detection of potential complications, allowing for swift medical intervention.
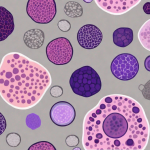
This empowerment extends to the realm of digital pathology and remote imaging, where advancements have streamlined the diagnosis process. Pathologists and oncologists can collaborate in real time, enhancing the accuracy of diagnoses and the efficiency of treatment planning. Similarly, remote imaging facilitates the sharing and review of medical images, bringing specialized expertise to the fingertips of those in remote locations.
Tele-Trials: A Leap Forward in Clinical Research
Clinical trials are the backbone of progress in cancer treatment, yet participation has often been hindered by geographical constraints. Telehealth is changing this narrative through tele-trials, which allow patients to engage in clinical research from the comfort of their homes. This not only expands the pool of potential participants but also ensures a more diverse representation in research, paving the way for more inclusive and effective treatment options.
The Impact of Telehealth on Patient Outcomes
The benefits of telehealth extend beyond convenience, significantly enhancing patient outcomes. Studies highlight its role in improving patient satisfaction, reducing hospitalizations, and elevating the quality of life. Early detection of recurrences or complications through telehealth interventions leads to timely treatments, improving survival rates and overall patient well-being.
Navigating Challenges and Best Practices
Despite its potential, the widespread adoption of telehealth in oncology faces hurdles, including concerns about privacy, security, and the digital divide. Addressing these challenges requires secure telehealth platforms, comprehensive training for healthcare providers, and efforts to ensure equitable access to technology.
Best practices for telehealth implementation include prioritizing patient privacy, promoting patient education, advocating for reimbursement parity, and continuously evaluating and improving telehealth programs to meet the evolving needs of cancer care.
Conclusion: Telehealth and the Future of Oncology
Telehealth is not just a temporary solution but a cornerstone of modern oncology, offering a new paradigm of care that is accessible, patient-centered, and efficient. As we continue to embrace and refine this technology, the promise of telehealth in bridging gaps, empowering patients, and enhancing outcomes shines brightly on the horizon of cancer care.