Radiotherapy has significantly evolved as a pivotal treatment for prostate cancer, offering non-invasive, targeted therapy with promising success rates. This advancement stems from technological progress, including intensity-modulated and image-guided radiation therapy, enhancing precision while sparing healthy tissue. Understanding the role of the prostate and the implications of prostate cancer is crucial, with symptoms often unnoticed until advanced stages. Factors like age, family history, and ethnicity influence risk, emphasizing the importance of early detection. Radiotherapy’s effectiveness varies by individual cases, with factors like tumor stage and overall health impacting outcomes. It’s compared favorably to surgery and hormone therapy, often used in combination for optimal results. This guide underscores radiotherapy’s role in improving survival and quality of life for prostate cancer patients, highlighting the importance of informed discussions with healthcare providers for personalized treatment plans.
Prostate cancer is a serious condition that affects thousands of men around the world. It can be a significant cause of concern and anxiety, as it involves the delicate prostate, a vital part of the male reproductive system. However, with advancements in medical technology, particularly in the field of radiotherapy, the treatment of prostate cancer has significantly improved. In this article, we will explore the various advancements and the efficacy of radiotherapy in the treatment of prostate cancer, providing you with valuable insight and reassurance.
Understanding Prostate Cancer
Before delving into the advancements and efficacy of radiotherapy, it is important to have a clear understanding of what prostate cancer entails. The prostate is a small gland located below the bladder and in front of the rectum. It plays a crucial role in the production of semen, which nourishes and transports sperm. Prostate cancer occurs when the cells in the prostate gland begin to grow and divide uncontrollably, forming a tumor.
Although the exact cause of prostate cancer is unknown, certain factors such as age, family history, and ethnicity can increase the risk. Early detection is key to successful treatment, which is why regular screenings and prompt medical attention are essential.
The Anatomy and Function of the Prostate
Before we delve into the details of radiotherapy, let’s take a moment to understand the anatomy and function of the prostate gland. The prostate is a small, walnut-sized gland located just below the bladder and in front of the rectum. Its primary function is to produce seminal fluid, which nourishes and transports sperm during ejaculation.
The prostate gland is composed of several lobes and is surrounded by muscles, nerves, and blood vessels. It is a delicate organ that requires careful consideration and precision during treatment.
Common Symptoms and Diagnosis of Prostate Cancer
Prostate cancer may not present any symptoms in its early stages or may cause symptoms similar to other noncancerous conditions, making it challenging to detect. However, as the cancer progresses, some common symptoms may include difficulty urinating, frequent urination (especially at night), blood in the urine or semen, pain or discomfort in the pelvic area, and erectile dysfunction.
If you experience any of these symptoms or have concerns about your prostate health, it is crucial to consult a healthcare professional who can perform a thorough examination and recommend appropriate diagnostic tests, such as a prostate-specific antigen (PSA) blood test or a digital rectal examination (DRE).
The Evolution of Radiotherapy
The treatment of prostate cancer has come a long way over the years, thanks to continuous advancements in medical technology. Radiotherapy, in particular, has played a significant role in revolutionizing prostate cancer treatment, improving outcomes, and enhancing the quality of life for patients.
Early Techniques and Limitations
In its early days, radiotherapy was primarily delivered through external beam radiation therapy, where high-energy X-rays were directed at the prostate gland from outside the body. While this technique offered effective tumor control, it also caused damage to nearby healthy tissues, resulting in unwanted side effects.
The limitations of early radiotherapy techniques included long treatment durations and the potential for cumulative toxicity. Moreover, the precision and accuracy of radiation delivery were not as refined as they are today. However, these pioneering approaches paved the way for the advancements that followed.
Modern Developments in Radiotherapy
Today, thanks to technological advancements and cutting-edge equipment, radiotherapy has become significantly more precise and targeted. One of the most remarkable developments is the introduction of intensity-modulated radiation therapy (IMRT). IMRT allows for the delivery of radiation in varying intensities, maximizing tumor control while minimizing damage to surrounding healthy tissues.
Another groundbreaking technique is image-guided radiation therapy (IGRT), which uses sophisticated imaging systems to track and adjust for any tumor movement during treatment. This ensures more accurate and effective radiation delivery, minimizing the risk of damage to neighboring organs.
The Science Behind Radiotherapy
To truly understand the advancements and efficacy of radiotherapy for prostate cancer, it is essential to comprehend the role of radiation in cancer treatment and the intricate process and mechanism behind radiotherapy itself.
The Role of Radiation in Cancer Treatment
Radiation therapy works by damaging the DNA within cancer cells, preventing their ability to multiply and grow. The radiation can be delivered externally or internally, depending on the specific treatment plan designed by the healthcare team. External beam radiation therapy involves directing high-energy beams precisely at the tumor, while internal radiation therapy, also known as brachytherapy, involves placing radioactive materials directly into or near the cancerous tissue.
By selectively targeting cancer cells, radiotherapy aims to destroy the tumor while minimizing harm to healthy tissues. The advancements in technology have greatly improved the accuracy and precision of radiation delivery, maximizing its effectiveness and minimizing side effects.
The Process and Mechanism of Radiotherapy
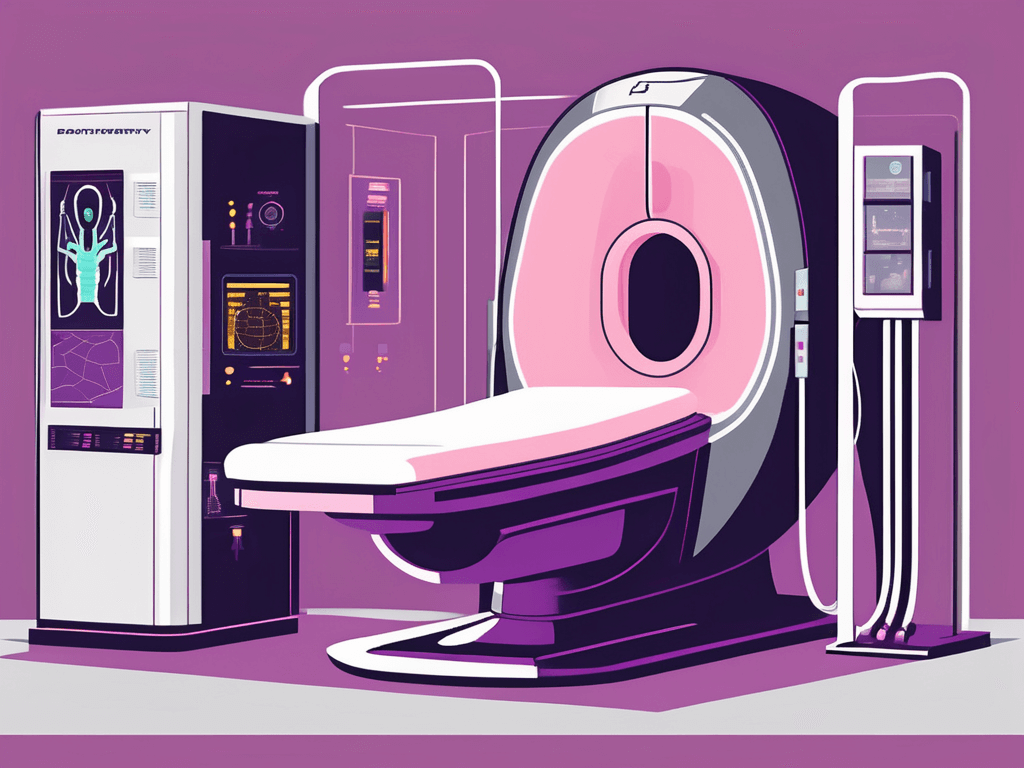
Radiotherapy is a carefully planned and executed treatment modality that involves multiple stages. The process typically begins with a comprehensive evaluation, including imaging scans and simulation sessions, where the exact position and shape of the tumor are determined.
During each radiotherapy session, you will be positioned comfortably on a specialized treatment table, and the radiation therapy team will ensure that you are in the correct position. The treatment machine will deliver the prescribed dose of radiation, and the entire process is painless and noninvasive.
Radiotherapy is typically administered over multiple sessions, with each session lasting only a few minutes. The total number of sessions will be determined by your healthcare team based on various factors, including the stage and aggressiveness of the cancer.
Efficacy of Radiotherapy in Prostate Cancer Treatment
When it comes to treating prostate cancer, radiotherapy has shown remarkable efficacy and positive outcomes. It offers a noninvasive and highly targeted approach to tumor control, providing patients with an excellent chance of long-term survival and improved quality of life.
Success Rates and Prognosis
The success rates of radiotherapy in the treatment of prostate cancer are impressive, with high cure rates reported in localized and locally advanced cases. Numerous studies have shown that patients who undergo radiotherapy experience excellent long-term disease control and improved overall survival rates.
It is important to note that the prognosis and success rates may vary depending on individual factors such as age, overall health, tumor stage, and response to treatment. Your healthcare team will thoroughly assess your specific case and provide you with personalized guidance and support throughout your treatment journey.
Factors Influencing Treatment Outcomes
While radiotherapy offers excellent prospects for prostate cancer treatment, it is important to understand that individual factors can influence treatment outcomes. These factors include tumor stage and grade, overall health status, presence of other medical conditions, and patient compliance with treatment protocols.
Your healthcare team will consider all these factors and tailor a treatment plan specifically for you, ensuring the best possible outcomes. It is crucial to maintain open and honest communication with your medical team, addressing any concerns or questions you may have along the way.
Comparing Radiotherapy with Other Treatment Options
When it comes to treating prostate cancer, radiotherapy is just one of several viable options. Comparing the benefits and potential drawbacks of different treatment modalities is crucial to making an informed decision that aligns with your unique needs and preferences.
Surgery versus Radiotherapy
Surgery, known as a radical prostatectomy, involves the complete removal of the prostate gland. While surgery can be an effective treatment option for certain cases, it is accompanied by potential risks and side effects such as incontinence and erectile dysfunction.
Radiotherapy, on the other hand, offers a noninvasive alternative to surgery, minimizing the risks of surgical complications and allowing for faster recovery. It is important to thoroughly discuss the pros and cons of both options with your healthcare team, considering factors such as tumor stage and your overall health status.
Hormone Therapy and Radiotherapy
Hormone therapy, also known as androgen deprivation therapy, is often used in conjunction with radiotherapy for the treatment of prostate cancer. It works by reducing the levels of testosterone in the body, as testosterone can stimulate the growth of prostate cancer cells.
Combining hormone therapy with radiotherapy has been shown to improve treatment effectiveness and outcomes, particularly in cases where the cancer has spread beyond the prostate gland. Your healthcare team will carefully evaluate your case and discuss the potential benefits of hormone therapy alongside radiotherapy.
In conclusion, the advancements and efficacy of radiotherapy in the treatment of prostate cancer have revolutionized the field of oncology. With modern techniques and precision delivery systems, radiotherapy offers remarkable tumor control while minimizing damage to healthy tissues. It is a highly effective and noninvasive treatment option that provides excellent long-term outcomes and improved quality of life. If you or a loved one are facing a prostate cancer diagnosis, consult with a healthcare professional who can guide you through the various treatment options, including radiotherapy, to develop an individualized plan that meets your specific needs.