Cancer cells, characterized by uncontrolled growth and the ability to invade tissues, are central to understanding and combating cancer. Their genetic mutations, resistance to cell death, and ability to evade the immune system make them formidable adversaries. These cells can spread to distant organs through metastasis and can become resistant to treatments, challenging the effectiveness of traditional therapies. Advances in cancer research, however, are uncovering new therapeutic targets and fostering personalized medicine approaches. By tailoring treatments to individual genetic profiles, we can improve responses and minimize side effects. This article delves into the characteristics of cancer cells, their role in disease progression, and their impact on treatment, highlighting the ongoing battle and future prospects in cancer research.
Cancer is a complex disease that affects millions of people worldwide. Understanding the role of cancer cells in disease progression is crucial for developing effective treatments and improving patient outcomes. In this article, we will delve into the unique characteristics of cancer cells, explore their role in disease initiation and progression, and discuss how they influence treatment response. By gaining a deeper understanding of cancer cells, we can work towards finding innovative approaches to combat this devastating disease.
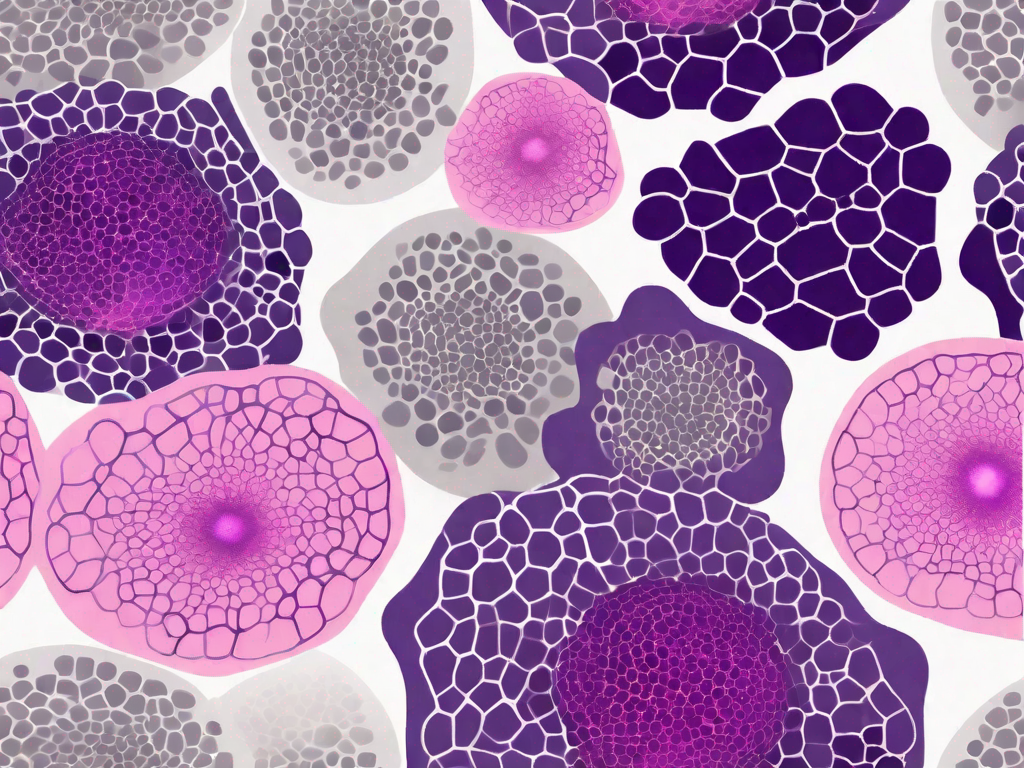
Defining Cancer Cells and their Unique Characteristics
Cancer cells are abnormal cells that divide uncontrollably and invade surrounding tissues. They differ from normal cells in several ways. One key characteristic is their genetic makeup. Cancer cells often harbor mutations in oncogenes, which promote cell growth, as well as tumor suppressor genes, which regulate cell division and prevent the formation of tumors.
Additionally, cancer cells possess a remarkable ability to adapt and survive in hostile environments. Unlike normal cells, which undergo programmed cell death (apoptosis) when they become damaged or dysfunctional, cancer cells can bypass this mechanism and continue to proliferate. This evasion of apoptosis allows cancer cells to persist and accumulate genetic alterations over time, leading to the development of more aggressive and resistant tumors.
Moreover, cancer cells exhibit a phenomenon known as angiogenesis, which is the formation of new blood vessels. This process is crucial for tumor growth and metastasis, as it ensures a constant supply of oxygen and nutrients to the expanding mass of cancer cells. Through the secretion of specific molecules, cancer cells can stimulate the growth of blood vessels from nearby tissues, creating a network that supports their survival and proliferation.
Furthermore, cancer cells have the ability to evade the body’s natural defense mechanisms. They can evade the immune system’s surveillance and develop strategies to avoid detection and destruction. For instance, cancer cells can alter the expression of certain proteins on their surface, making them less recognizable to immune cells. They can also release immunosuppressive molecules that inhibit the activity of immune cells, further dampening the immune response against them.
Additionally, cancer cells exhibit a high degree of heterogeneity, meaning that they can vary in their genetic and phenotypic characteristics within a single tumor. This heterogeneity contributes to the complexity of cancer and poses challenges for its treatment. Different subpopulations of cancer cells may have distinct vulnerabilities and resistance mechanisms, making it difficult to target the entire tumor with a single therapeutic approach.
Overall, the unique characteristics of cancer cells, including their genetic alterations, evasion of apoptosis, angiogenesis, immune evasion, and heterogeneity, contribute to the aggressive nature of cancer and its ability to spread throughout the body. Understanding these characteristics is crucial for developing effective strategies to diagnose, treat, and prevent cancer.
The Role of Cancer Cells in Disease Initiation
Disease initiation occurs when normal cells undergo a process called cellular transformation, acquiring genetic alterations that enable them to become cancer cells. This transformation can be triggered by various factors, such as exposure to carcinogens, genetic predisposition, or viral infections.
Oncogenes and tumor suppressor genes play a crucial role in cellular transformation. Oncogenes are cancer-causing genes that promote cell growth and division. When these genes become mutated or activated, they lead to uncontrolled cell proliferation and the formation of tumors. In contrast, tumor suppressor genes regulate cell growth and prevent the development of tumors. However, mutations in these genes can impair their function, allowing cancer cells to evade growth control mechanisms.
Exposure to carcinogens is a significant risk factor for cellular transformation and the initiation of cancer. Carcinogens are substances or agents that can cause genetic alterations in normal cells, leading to their transformation into cancer cells. These substances can be found in various environmental factors, such as tobacco smoke, certain chemicals, radiation, and even some foods. When normal cells are exposed to these carcinogens, their DNA can be damaged, resulting in the activation of oncogenes or the inactivation of tumor suppressor genes.
Genetic predisposition also plays a role in disease initiation. Some individuals may inherit genetic mutations that increase their susceptibility to cancer development. These mutations can be present in oncogenes or tumor suppressor genes, making individuals more prone to cellular transformation. For example, individuals with mutations in the BRCA1 or BRCA2 genes have a higher risk of developing breast and ovarian cancer.
Viral infections can also contribute to disease initiation. Certain viruses, such as human papillomavirus (HPV), hepatitis B virus (HBV), and human immunodeficiency virus (HIV), have been linked to the development of specific types of cancer. These viruses can infect normal cells and introduce their genetic material, which can disrupt the normal cellular processes and lead to cellular transformation. For instance, HPV infection is a major risk factor for cervical cancer.
Once cellular transformation occurs, cancer cells acquire several characteristics that distinguish them from normal cells. These characteristics include uncontrolled cell growth, evasion of cell death mechanisms, the ability to invade surrounding tissues, and the ability to spread to distant sites in the body (metastasis). Cancer cells also have the ability to induce the formation of new blood vessels (angiogenesis), which provides them with nutrients and oxygen to support their growth and survival.
In conclusion, the role of cancer cells in disease initiation is complex and multifactorial. It involves the acquisition of genetic alterations through exposure to carcinogens, genetic predisposition, or viral infections. Oncogenes and tumor suppressor genes play a crucial role in cellular transformation, leading to uncontrolled cell growth and the formation of tumors. Understanding the mechanisms underlying disease initiation is essential for developing effective strategies for cancer prevention and treatment.
Cancer Cells and Disease Progression
Once cancer cells have initiated the disease, their ability to metastasize and spread to distant sites becomes a major concern. Metastasis is a complex process involving the detachment of cancer cells from the primary tumor, invasion into nearby tissues, entry into the bloodstream or lymphatic system, and colonization of distant organs.
Furthermore, cancer cells can exert a detrimental impact on the immune system. They can evade immune detection by downregulating the expression of certain molecules that are recognized by immune cells. This evasion allows cancer cells to continue proliferating and spreading throughout the body.
The Influence of Cancer Cells on Treatment Response
Treating cancer is a complex task, often complicated by the inherent ability of cancer cells to develop resistance to therapy. Drug resistance occurs when cancer cells adapt and become less responsive to treatment, leading to treatment failure.
The development of drug resistance involves various mechanisms. Some cancer cells possess specific genetic alterations that enable them to neutralize the effects of treatment drugs. Additionally, cancer stem cells, which are a small population of cells with the ability to self-renew and differentiate, have been implicated in treatment resistance. These cells can survive conventional therapies and give rise to new tumors, contributing to disease recurrence and progression.
Future Perspectives in Cancer Research
Despite the challenges posed by cancer cells, researchers are making significant strides in the field of cancer research. Exciting new therapeutic targets are being identified, opening up possibilities for novel treatments.
Personalized medicine is also gaining traction in cancer treatment. By tailoring therapies to an individual’s unique genetic makeup, it is possible to achieve better treatment responses and minimize side effects. This approach holds promise for enhancing patient outcomes in the future.
Conclusion
Understanding the role of cancer cells in disease progression is vital for improving our ability to diagnose, treat, and prevent cancer. By delineating the unique characteristics of cancer cells, elucidating their role in disease initiation and progression, and exploring their influence on treatment response, we can make significant strides in the battle against this devastating disease. Through continued research and innovation, we can work towards a future where cancer is no longer a life-threatening diagnosis but a manageable condition.